Introduction
Clinical trials are pivotal for developing new medical treatments and advancing scientific understanding. However, the traditional clinical trial model is fraught with challenges such as slow patient recruitment, uneven retention rates, and limited participant diversity. The emergence of digital health technology is rapidly transforming these processes, bringing clinical research closer to patients and making participation more feasible than ever. Initiatives like BioNTech clinical trials exemplify how technological adoption is changing the clinical landscape and redefining what is possible for participant access and experience in research.
As digital tools break down historical barriers, more patients can join studies from remote locations, and researchers gain richer, real-time data. Artificial intelligence, machine learning, and wearables are now mainstream in innovative trial designs that facilitate patient engagement, while decentralized and hybrid models continue to expand their reach. Participant-centric clinical research is becoming the norm through these advances, opening doors for faster breakthroughs and more representative results.
This evolution in methodology is not just about convenience; it’s a critical leap forward for inclusivity and scientific rigor. By leveraging cutting-edge digital solutions, sponsors, investigators, and regulatory bodies can collectively improve trial efficiency and patient outcomes. Alongside these benefits, there is increased attention on ethical guidelines, data privacy, and the need for greater health equity—a necessary focus as more clinical trials pivot to technology-based participation.
With the post-pandemic acceleration of virtual capabilities, staying informed on the future trends in clinical research is vital for patients, healthcare providers, and the broader scientific community. To further explore the wider implications, the National Center for Advancing Translational Sciences (NCATS) outlines the potential of technology in expanding access to research through digital and decentralized trial approaches.
The Rise of Decentralized Clinical Trials
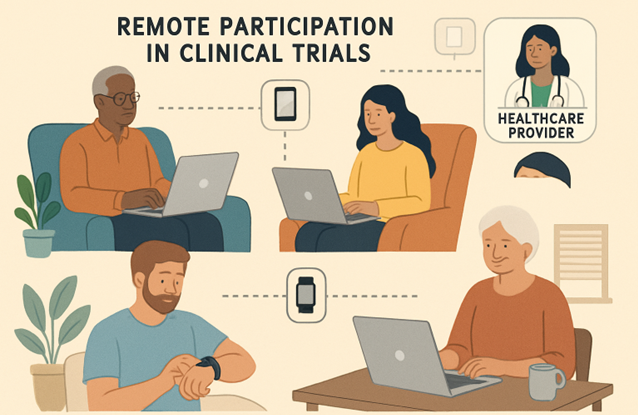
Decentralized clinical trials (DCTs) are innovating the research space by shifting activities away from traditional study centers into patient homes and communities. By using secure web platforms, telemedicine, direct-to-patient shipments, and remote diagnostics, DCTs minimize participants’ travel burdens and logistical complexities. This democratized approach increases participation among those who may have been excluded by distance, health limitations, or inflexible work schedules, and it ensures that trial populations more closely represent real-world patient demographics.
The COVID-19 pandemic accelerated the need for scalable remote solutions, and sponsors quickly adopted virtual visits and electronic consent. According to a report by Nature, decentralized models have reduced start-up timelines and improved patient engagement, highlighting that the shift is likely to persist beyond the pandemic as a new gold standard for research flexibility and accessibility.
AI and Machine Learning in Patient Recruitment
Integrating artificial intelligence (AI) and machine learning into clinical trial operations streamlines what has historically been one of the most challenging phases—finding and enrolling eligible participants. AI-driven systems can mine electronic health records, social media, and insurance databases to identify patients who meet complex study criteria. Natural language processing further accelerates screening and matches individuals across vast data points, making recruitment more targeted and less labor-intensive for sites.
Personalization and Predictive Analytics
Machine learning also enables predictive analytics, providing insights into which prospective participants will likely complete a trial, thus improving retention rates. This tailored approach ensures trials are more efficient, while also helping to address issues of underrepresentation by flagging opportunities to recruit diverse subgroups.
Wearable Technology and Remote Monitoring
Wearables and connected home medical devices are transformative in today’s clinical trials. Smartwatches, glucose monitors, and biosensors allow continuous, real-time data collection without frequent in-person visits. This remote monitoring generates richer datasets, reduces recall bias, and enhances patient safety by enabling quicker responses to adverse events.
According to The Wall Street Journal, integrating such technologies in clinical research improves both compliance and retention while offering participants the convenience of contributing to science from their everyday lives. Wearables also drive the shift toward more patient-centered protocols, tailoring interventions based on individualized data.
Enhancing Diversity in Clinical Trials
Diversity in clinical research is crucial to ensure treatments are effective for all populations. Emerging technologies tackle long-standing barriers—like language, transportation, and time commitments—by facilitating virtual visits, multilingual platforms, and flexible participation options. These advances attract participants from traditionally underrepresented groups and help address disparities in health outcomes.
Inclusive Recruitment Strategies
Sponsors and advocacy groups now utilize community outreach, social media, and AI-driven targeted advertising to improve awareness and inclusion. These proactive strategies are helping clinical trials become more representative of real-world patient populations, strengthening the validity and applicability of research findings.
Regulatory Changes and Guidelines
To keep pace with digital evolution, regulatory agencies, including the FDA and EMA, are updating their frameworks to support technology-driven research while maintaining patient safety and trial integrity. Developing new guidelines for e-consent, remote monitoring, and decentralized operations underscores the need for robust data security, ethical conduct, and transparency throughout the trial process.
These regulatory adaptations enable sponsors to implement innovative designs, provided they maintain compliance and uphold the rigor associated with clinical research. Continued international collaboration among regulators is essential as technology blurs traditional geographical lines, creating opportunities for truly global studies and harmonized standards.
Challenges and Considerations
Despite the significant advancements, several challenges persist. Digital health literacy varies widely, and not all populations have equal access to high-speed internet or personal devices required for participation. Data security and patient privacy require sophisticated cybersecurity measures and transparent consent processes.
It is also crucial to address potential biases in AI algorithms, ensuring fair recruitment and preventing the exclusion of certain groups. Continuous oversight, education, and investments in infrastructure are necessary to bridge the digital divide and ensure equitable access for all participants.
Conclusion
Integrating technology into clinical trials reshapes research by making it more accessible, representative, and efficient. As the industry embraces these innovations, it is essential to prioritize equity, privacy, and adaptability to meet the diverse needs of future patient populations. The intersection of digital health and clinical research holds immense promise for accelerating medical breakthroughs and improving public health outcomes worldwide.